Hi, my name is Allison Schaaf. My own fertility journey, including five miscarriages, inspired me to create this website to help you navigate your fertility path.
Here are my main takeaways I would share with you as a friend:
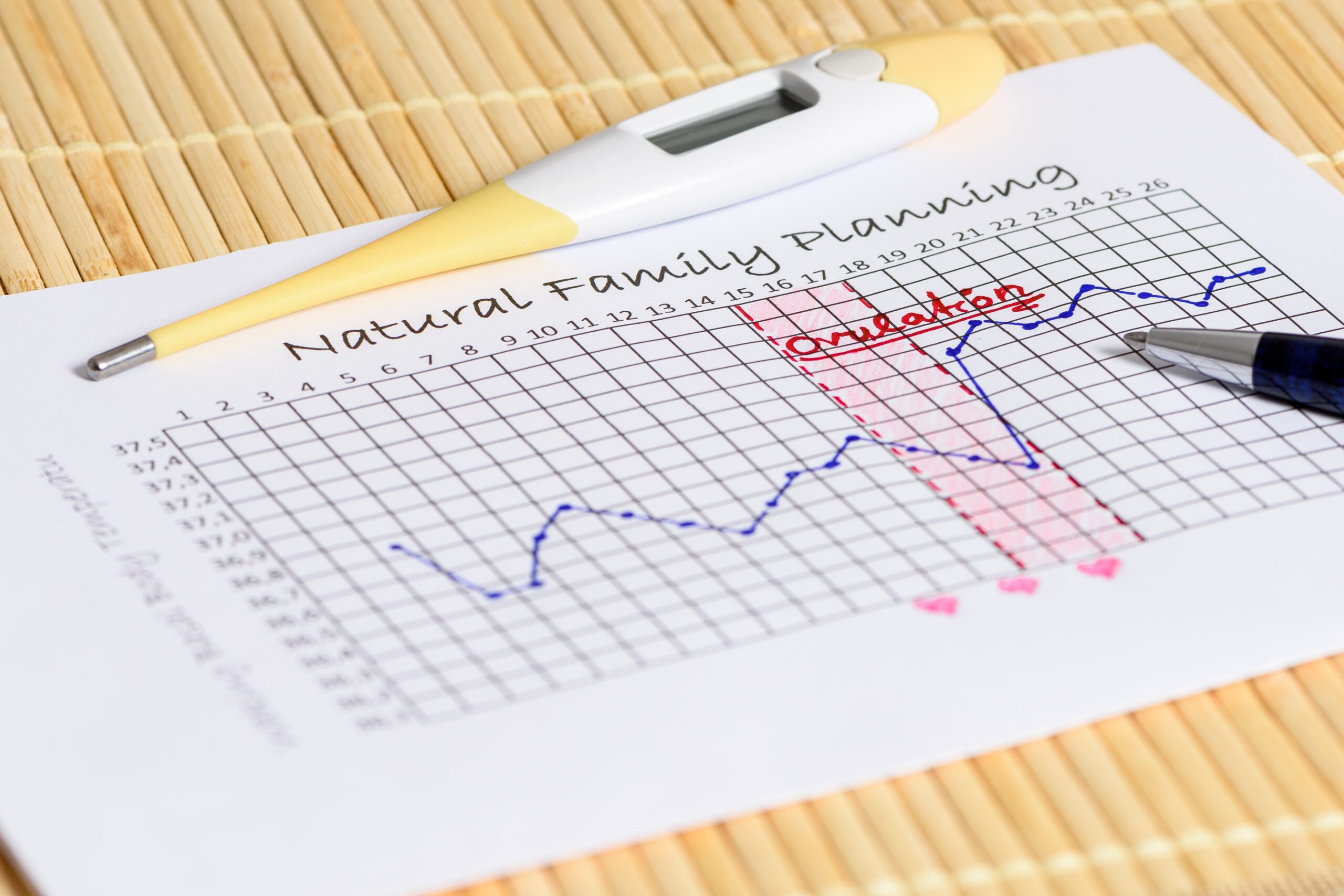
- Tracking specific metrics such as basal body temperature and LH levels can help you better predict when you will ovulate.
- There is a wide range of devices available to help you better track and predict your ovulation. These convenient devices can take the guesswork out of timing intercourse to result in pregnancy.
- Tracking and understanding your cycle is an important step toward taking control of your fertility.
I also recommend you do your own research and work with your doctor. That is why I have coordinated these articles with the nitty-gritty details and links to research so you can make an informed decision on what works best for you… read on for more! And—don’t miss my Next Steps section at the bottom.
What is ovulation tracking?
Basal body temperature (BBT) tracking
What are the factors that affect basal body temperature?
Miscarriage and basal body temperature
How does basal body temperature tracking work?
Other Ways to Track Fertility and Ovulation
When is the best time to get pregnant?
If you’ve had a miscarriage or multiple miscarriages, the idea of getting pregnant again can be scary. Understandably, you want to get everything right to achieve a successful pregnancy.
Because every woman is different, we’re all slightly different in how our biology varies throughout the menstrual cycle. Sensibly, researchers are still working towards the best non-invasive way to reliably predict ovulation. Existing methods combine different hormone tests with signs and symptoms, even using artificial intelligence. Ovulation prediction becomes even more challenging in women with irregular cycles or fertility concerns 1.
The best way to determine when you ovulate is to learn about how your body changes through each cycle by combining multiple methods to maximize your chance of getting pregnant. This article, part 1, will cover how your body changes throughout your cycle, the science behind ovulation tracking, different methods you can use, and their pros and cons 2 In Part II, we’ll cover fertility tracker, devices, home tests, and apps you can use to make tracking and finding your fertile window easier.
What is ovulation tracking?
Ovulation tracking refers to ways to identify your fertile window when you’re most likely to become pregnant. The fertile window consists of about six days when sexual intercourse can lead to pregnancy during an average menstrual cycle. These six days include 5, 4, 3, 2, 1 days before ovulation and the day ovulation occurs 3.
If your cycles have been irregular or you occasionally skip ovulation, ovulation tracking becomes even more important to help you conceive. Also, it can provide helpful feedback if you’re making lifestyle changes to balance your hormones and improve your fertility.
Now, let’s first understand how your body changes throughout each cycle and the signs you can use to track ovulation.
Hormonal changes during a menstrual cycle: A primer
During each menstrual cycle, your body prepares an egg for fertilization and your uterus for embryo implantation 4.
Your ovaries have many developing follicles that respond to follicle-stimulating hormones (FSH) from the pituitary gland in your brain. The follicles secrete estrogen, which in turn reduces FSH production.
During this process, a follicle gets selected naturally, becomes dominant, and grows. Meanwhile, other adjacent follicles degenerate due to decreasing levels of FSH. The dominant follicle continues to secrete estrogen. Sufficiently high estrogen triggers the pituitary gland to abruptly release luteinizing hormone (LH), and this surge in LH triggers ovulation.5
Ovulation is when the egg is released from the follicle.
After ovulation, the dominant follicle becomes a corpus luteum. It secretes progesterone and estrogen before finally disintegrating, initiating menstruation.6
Progesterone and estrogen affect many other aspects of your physiology, such as your body temperature. You can find your fertile window based on these hormonal and physical changes.
Basal body temperature (BBT) tracking
Monitoring and tracking BBT is one of the least invasive and simplest methods to track ovulation.
What is basal body temperature?
Basal body temperature (BBT) is your body’s temperature when you are entirely at rest. It is the core body temperature, which is measured under the tongue, rectally, or in the armpit.
Most women will have a slight increase in their normal body temperature during ovulation by about 0.5 to 1oF. The body temperature may remain elevated until menstruation or a few days prior 7
You can use basal body temperature to maximize your chance of getting pregnant. However, since many factors influence your BBT, BBT tracking is not a reliable contraceptive method 8.
However, combining BBT tracking with other pieces of information (see other methods below) can increase its accuracy.
What are normal basal body temperatures during the follicular phase, luteal phase, and pregnancy?
Before ovulation, your basal body temperature remains low, usually ranging from 97.0 to 98.0° F. Approximately one day before ovulation, you will have a dip in the BBT, where it reaches its lowest point.
Once ovulation occurs, the corpus luteum secretes progesterone, increasing your basal body temperature by about 0.5 to 1.0 °F. This change in BBT suggests that ovulation has occurred.91011 The BBT then stays elevated throughout the luteal stage of the menstrual cycle. BBT usually ranges between 97.6 and 98.6°F after ovulation during the luteal phase.
During the latter part of the luteal stage, the corpus luteum degenerates, decreasing the serum progesterone levels. Therefore, the basal body temperature returns to the preovulatory level either one to two days before or immediately at the start of menstrual bleeding.
If you get pregnant and miss your period, the BBT will remain elevated during the entire luteal phase. This is an excellent and accurate sign of pregnancy. 12
During pregnancy, the BBT tends to stay above 98.4°F consistently with daily fluctuations of less than 0.4°F. It may even rise consistently during your first trimester of pregnancy.
After the first trimester, the corpus luteum breaks down, and the placenta takes over to help produce progesterone. In typical pregnancies, the switchover to the placenta can cause the BBT to drop by about 0.5°F once you reach the second trimester and by 0.2°F per month afterwards.1314
What are the factors that affect basal body temperature?1516
The various factors that may influence basal body temperature include:
- Fever due to an infection
- Hypothyroidism can decrease BBT, whereas hyperthyroidism can increase it 17
- Physical or emotional stress
- Luteal phase defect may cause a less sharp increase in BBT during the luteal phase 18
- Drug or alcohol use
- Sleep disturbance/lack of sleep
- Change of your waking time
- Changes in the room temperature
- Starting or discontinuing birth control pills (BCPs)
- Medications that affect body temperature, such as fever medications
- Change of weather
- Travel
- Indigestion
- Sexual intercourse
- Exercise
- Certain medical disorders
Miscarriage and basal body temperature
During pregnancy, the basal body temperature won’t return to normal preovulatory levels. It continues to rise somewhat during the first trimester of pregnancy because the corpus luteum is producing high levels of progesterone.
In women with a history of early recurrent miscarriage, a decline in BBT or subnormal levels may indicate inadequate progesterone production, indicating a threatened or spontaneous miscarriage and fetal demise. This information is very useful in managing early pregnancy as your doctor may test and prescribe progesterone.1920
How does basal body temperature tracking work?
After charting your BBT for a few cycles, you may notice patterns unique to your body. You can also identify ovulation based on your pattern. The steps mentioned below may help you start tracking your basal body temperature and determine the time of ovulation.
Step 1: Use a glass or digital basal thermometer with two decimal points to have the necessary accuracy in detecting small rises in BBT. Measure your basal body temperature orally every morning before getting out of bed.
Note: technically, the BBT can also be measured rectally and in the armpit to accurately measure core body temperature. However, devices that take temperature away from your body, such as on your wrist or fingers, do not measure core body temperature. These devices may detect the relative increase in body temperature but cannot measure BBT accurately.
Step 2: Record the temperature on the fertility or ovulation tracking calendar or app each day.
Step 3: When you record your temperature every day during a menstrual cycle, you will notice the BBT is almost consistent before ovulation. As the day of ovulation comes nearer, you may observe a slight decline followed by an abrupt increase in the BBT after ovulation. This increase in temperature is an indication of ovulation.
Some points you should take care of while measuring basal body temperature are:
- Since the BBT reading may get affected by lack of sleep, it is vital to sleep for a minimum of three consecutive hours before measuring it.
- Measure your temperature at the same time each day; the ideal time is before getting out of bed in the morning.
- Measure your temperature from the same place each day. You can take it from your vagina or mouth.
As the chart evolves gradually, you will start noticing a pattern. Each woman’s pattern is different but may also vary in the same woman from one menstrual cycle to another. Therefore, you should record your temperature and chart your cycle for a few months to get accustomed to your fertile window patterns. 21
The temperature shift is quite subtle, so the only way to learn about your body is by charting it out daily throughout your menstrual cycle. That way, you can recognize this shift to pinpoint the ovulation time.22
Using a combination of BBT and progesterone levels helps to indicate a healthy pregnancy. For example, Dr. Reena Singh ND of Zama Wellness will use a combination of BBT and progesterone levels to indicate a need for supplemental progesterone, or not. The naturopathic optimal range of progesterone is over 28 ng/mL at 6 weeks of pregnancy 23.
Other Ways to Track Fertility and Ovulation
1. Ultrasound
Transvaginal ultrasound helps define the ovulation time and is the standard reference method to detect ovulation. Experienced radiologists, technicians, or gynecologists perform transvaginal ultrasounds.
The ultrasound detects the maximum size of the dominant follicle and its subsequent size reduction. It can tell when ovulation occurs in between when the follicle grows and shrinks. It is not routinely used since it is inconvenient, expensive, and invasive. However, ultrasound is the ovulation detection technique of choice for fertility treatments 24.
2. Luteinizing hormone surge
Detection of an increase in the luteinizing hormone (LH) in the urine or serum is a very specific and sensitive method of ovulation tracking. It provides significant accuracy in determining your conception capacity.
LH starts to surge at about 35 to 44 hours before ovulation. The LH level reaches its peak about 10 to 12 hours before ovulation. You can test it with urine strips or get a blood draw.
Every woman and every cycle is different, so it’s a good idea to learn about your body by tracking your LH throughout multiple menstrual cycles. This can help you accurately estimate your fertile window and ovulation time once you’re TTC.
Beginning from day 10 to 11 of a new menstrual cycle (day one of menstrual bleeding is the first day of your menstrual cycle) or four days prior to the estimated day of ovulation, you may test your urinary luteinizing hormone once or twice a day.
Highly sensitive urinary LH kits may detect concentrations of LH as low as 22 mlU/ml. The natural increase in LH levels in urine may range from 20 to 100 mlU/ml. 25
3. Progesterone levels
Once ovulation occurs, the dominant follicle converts into a corpus luteum that secretes progesterone. To confirm ovulation, measure the levels of progesterone in the serum, saliva, or urine.
Blood progesterone measures progesterone being transported, whereas salivary progesterone measures the hormone levels between cells, which are more reflective of active hormones. Urinary progesterone measures the progesterone that your body is eliminating after use.
If your progesterone is 5 ng/ml or more, there is a 98.4% chance you ovulated. However, about 10.4% of women ovulated but with their progesterone was still lower than 5 ng/mL. 26
4. Urinary Pregnanediol Glucuronide (PdG)
Pregnanediol glucuronide (PdG) is a breakdown product of progesterone. PDG may only become detectable in the urine once progesterone hits a certain threshold, which is why it’s helpful to indicate ovulation and luteal phase defect.
Naturally, your ovaries and adrenals secrete PdG in pulses. Then, your liver converts it into PdG before your body eliminates the PdG in the urine. While levels of PdG correlate with progesterone levels, it’s more representative of your average progesterone production in a span of a few hours. In the urine PdG levels are 1,000 – 4,000 times greater than progesterone levels. 27
Water intake can affect the concentration of all metabolites in the urine, so studies found that PdG tests are only valid when the urine is more concentrated (specific gravity over 1.015). So, morning urine, which is more concentrated, is best for testing PdG levels.28
There are a few small clinical trials that compare PdG with other methods. They found that the PdG rise has 100% specificity to ovulation, but 85-88% sensitivity 29 30. That means when a PdG goes up, ovulation certainly has occurred, but not all ovulation results in a sufficient increase in PdG for the test to detect. About 12-15% of true ovulation cases may be missed if only the PdG test is used since factors such as aging can reduce progesterone. However, its accuracy increases when other fertility markers are taken into account.
In a BioCyc study involving 259 women, they found that a urinary estrogen metabolite and PdG are good proxy for ovulation because they have a strong concordance with LH peak. 31
In a clinical study using the PdG measurement strips, they found that once PdG reaches over 5 mcg/mL for 3 mornings in a row, 100% of subjects ovulated as confirmed by transvaginal ultrasound and LH tests. However, only about 80% of women who ovulated had sufficient PdG for the tests to detect 32. This study used the Proov test, which is currently the only commercially available test that measures PdG.
Continual PdG rise after ovulation may predict conception and pregnancy outcomes. In a study of 347 female textile workers, the drop in PdG on days 5-9 after ovulation seemed to indicate non-conception or early pregnancy loss. However, the number of subjects in this study was too small to develop into any type of early diagnostic test 33.
Image source:34, Caption: PdG at 5 -10 days post ovulation may predict conception and pregnancy outcomes.
Currently, the only company that provides PdG tests is Proov. They provide test strips that change colors if the PdG is above a threshold at 5 mcg/mL, along with an app that tracks PdG levels by taking a photo of a test strip.
You can use the code MHD is for to take 20% off the following tests and products: Confirm PdG tests, Predict & Confirm, Predict LH tests, Assess FSH tests, Balancing Oil, and Luteal Love kits.
Factors that may interfere with PdG measurement include:
- Premature ovarian insufficiency may raise PdG by 2-3 times as the adrenals start to compensate with progesterone production 35. However, the higher PdG in this scenario does not mean better fertility.
- Progesterone therapy can make PdG more variable and thus less reliable 36.
5. Cervical mucus
The endocervical and cervical glands secrete the cervical mucus that helps transport the egg and select sperm once the egg is ready. Mucus appearance and consistency vary during different menstrual cycle stages.
During the follicular stage of your menstrual cycle, the cervical mucus is scanty, viscous, and thick, forming a barrier to the entrance of sperm before the egg is ready. You will have more abundant cervical mucus around ovulation. The mucus also becomes clearer, more watery, and has an egg-white consistency.
Observation of cervical mucus is one of the cheapest methods of tracking ovulation. You may collect mucus from your vagina with two fingers or observe cervical mucus present at the vulva externally. 37
The peak day (PD) of cervical mucus is a significant biological marker when determining the ideal time of fertility during a female’s menstrual cycle. Studies show that the peak day of cervical mucus is an accurate method of determining optimal fertility and ovulation day, which coincides with the LH surge. 38
6. Salivary ferning and analysis
Increasing adrenocorticotropic hormone and estrogen levels before ovulation stimulates aldosterone secretion that helps regulate the status of fluid and electrolytes in the human body. Estrogen causes the crystallization of NaCl; this appears as fern leaves in the saliva under the microscope 39 40 41
Observation of a ferning pattern under a microscope at the time of ovulation was initially described by Dr. Biel Cassal in 1968. The biological behavior of saliva is similar to cervical mucus in its increased response to raised levels of estrogen.
The salivary ferning method is a non-invasive and cost-effective diagnostic procedure for determining the time of ovulation. It is advantageous over hormonal estimation and measuring basal body temperature. However, basal body temperature and salivary ferning method together may be more useful to indicate the fertility status. You may do the ferning method at home using a handheld microscope. 42
When is the best time to get pregnant?
The fertile window consists of approximately five days before you ovulate and the day when ovulation occurs during each menstrual cycle. 43
If your periods are regular and you desire to conceive, the best time to conceive is one day before ovulation. However, the chances of conceiving are also good during your entire ‘fertile window.’ The more frequently you have sexual intercourse during this fertile window, the greater your chances are of becoming pregnant.
Sperm has a short lifespan in the female reproductive tract and may become less viable over time, although it may last up to five days. So, the more times you try, the higher the chance you will have fresh sperm available while you ovulate. 44. These fertility tracking methods make it easier for you to learn about your body and identify your fertile window. That way, you can maximize your chance of getting pregnant and reaching full-term.
In Part II, we cover fertility and ovulation tracking technologies.
Next Steps to Consider
- Ask your doctor about what tracking method might be most appropriate for you.
- Consider purchasing a device to help track ovulation.
- Download our free lab tracker for more testing to consider if you are experiencing recurrent miscarriages.
- Check out our progesterone article to learn more about the hormone, what it does in the body, and how to support your progesterone levels
Note: This article may contain affiliate links. We appreciate your support of Miscarriage Hope Desk!
References


0 Comments