Hi, my name is Allison Schaaf, my own fertility journey, including 5 miscarriages, inspired me to create this website to help YOU navigate your own fertility journey.
Here are my main takeaways I would share with you as a friend:
- Genetic causes contribute to a significant number of miscarriages, however, recurrent miscarriages are more likely due to non-genetic causes
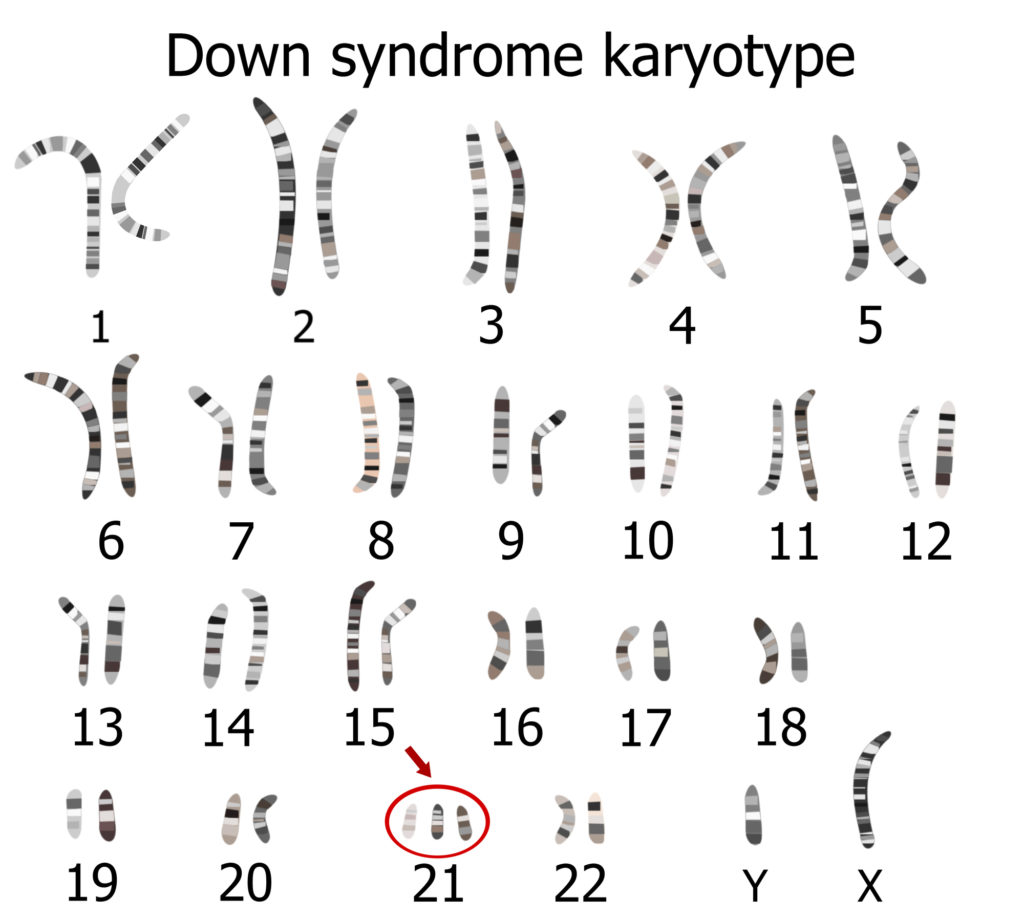
- Testing for potential genetic issues (through karoytyping or other advanced testing) may help uncover causes of miscarriages
- While some risk factors for chromosomal anomalies are out of your control, there are risk factors you can control for
Of course, I also recommend you do your own research! That is why I have coordinated these articles with the nitty-gritty details and links to research so you can best decide what works best for you, read on for more! And don’t miss my Action Steps at the bottom of the article!
Table of Contents
How chromosomal and genetic abnormalities lead to miscarriages
Types of chromosomal abnormalities that lead to miscarriages
What causes chromosomal anomalies?
Should you get genetic testing?
Genetic causes, including chromosomal anomalies, may contribute to over 90% of miscarriages before the 8th week, 50% between weeks 8 – 11, and 30% between weeks 16 – 191. However, recurrent miscarriages are more likely to be due to non-genetic causes, so only around 30 – 50% of these are due to chromosomal causes2.
Fortunately, once the genetic causes of miscarriages are determined and addressed, many couples go on to have successful pregnancies. Also, technologies such as preimplantation genetic testing and fertility treatments can help select embryos without chromosomal damages. Overall, couples who have had miscarriages from genetic causes have a better outlook than those who had miscarriages due to other causes3.
This article will cover different genetic causes of miscarriage and ways to address them. In our genetic testing article, you can learn about different genetic testing options available.
How chromosomal and genetic abnormalities lead to miscarriages
Genetic mutations, including chromosomal abnormalities, can disrupt gene function. It can cause miscarriage if the disrupted genes are important for embryonic development. These disruptions can stop embryonic development, leading to miscarriages. The mother’s immune system may also recognize these developmental problems and end the pregnancy4.
Most genetic abnormalities found in embryos arise from mistakes during the creation of egg and sperm cells, or soon after fertilization. These abnormalities, which contribute to the majority of early miscarriages, are random and don’t tend to happen again. Many root causes of these random mutations can be addressed through diet and lifestyle changes.
In some cases, especially with recurrent miscarriages, one or both parents could be a genetic carrier for variants that contribute to the miscarriage. For example, chromosomal translocations are found in up to 5% of couples with recurrent pregnancy loss5. Fortunately, most of these couples end up with healthy pregnancies.
Types of chromosomal abnormalities that lead to miscarriages
Introduction to human genetics and chromosomal abnormalities
Chromosomes are structures that hold your main DNA. The DNA is wound around globular proteins called histones. The DNA sequence contains 4 different types of nucleotides: adenine (A), guanine (G), cytosine (C), and thymine (T). The order of these nucleotides encodes your genes. A genome is the composition of an entire set of chromosomes, including DNA and genes in a human (~23,000 genes, one copy from each parent).
Humans have 23 pairs (46 in total) chromosomes in most of our cells, with the exception of sperms and eggs. 1 pair is called the sex chromosome, which could be XX in females and XY in males. The remaining 22 pairs are “autosomes.” The sperms and eggs have 23 unpaired chromosomes, including one sex chromosome in each cell. All eggs have 22 + X, and sperms could be 22 + X or 22 + Y, each denoting 22 autosomes and one sex chromosome.
An addition of one chromosome is called a trisomy, whereas a subtraction of one chromosome is called a monosomy. Polyploidy refers to gaining entire sets of chromosomes. Having an extra set of chromosomes (3 total sets) is called “triploidy,” whereas having two extra sets of chromosomes (4 total sets) is called tetraploidy.
Among miscarried cases where the product of conceptions was available for analysis, the most common numerical chromosomal abnormality is trisomy (61.2%), followed by triploidy (12.4%), monosomy X (10.5%), tetraploidy (9.2%), and structural chromosomal anomalies (4.7%)6.
These genetic abnormalities can be present in all cells, or some cells (mosaicism). The percentage of mosaicism tells you how many percent of an embryo’s cells carry the genetic anomalies. A high percentage may increase the chance of miscarriage, whereas a low percentage can either contribute to some milder pregnancy complications or no complications at all.
Most of these chromosomal anomalies happen during the production of eggs and sperms, or during fertilization. However, in rare cases, especially with recurrent miscarriages, the parents may be carriers of chromosomal translocation.
Incorrect chromosome numbers (aneuploidy)
Numeric aberrations are when the fetus has an incorrect number of chromosomes, which could be more or less than 46 chromosomes. These can be called collectively “aneuploidy.”
Early in your pregnancy, your physician may recommend a blood test called non-invasive prenatal testing (NIPT) to screen for potential aneuploidies. However, keep in mind that this is a non-invasive screening test that is not always correct. If NIPT has significant findings, you will need a more accurate test of fetal genetic material in the amniotic sample to confirm the results.
1) Trisomy – having an extra copy of a chromosome
Normally, an embryo should have a pair of each chromosome. Having an extra one of a chromosome is referred to as trisomy, resulting in a total of 47 chromosomes.
Among miscarried trisomies, chromosome 16 (21.8%), 22 (17.9%), and 21 (10%) were most frequently found7. Abnormalities in chromosomes 13, 18, X and Y are also frequently found8. Embryos with these trisomies tend to die early, although some of them do develop full-term. Those that survive may suffer from multiple congenital health problems, such as:
- Down’s syndrome – an extra chromosome 21
- Patau’s syndrome – an extra chromosome 18
- Edward’s syndrome – an extra chromosome 13
Trisomies 21, 18, and 13 are most likely to survive a full-term pregnancy.
A trisomy can be9:
- Full trisomy – the embryo has an entire extra chromosome
- Partial trisomy – there is an extra part of a chromosome
- Secondary trisomy – if the chromosome has extra identical arms
- Monosomy – losing one chromosome
2) Monosomy – losing one chromosome
An embryo that misses one chromosome has monosomy, resulting in a total of 45 chromosomes in their cells. The most common one is monosomy X. In females, it leads to Turner’s syndrome, where the child has short stature, early ovarian dysfunction, and infertility10.
3) Polyploidy – extra full sets of chromosome
Polyploidy is when the embryo has one or multiple extra sets of chromosomes, typically resulting in a total of 69 (triploidy) or 92 (tetraploidy) chromosomes. This type of chromosomal anomalies may happen in cell divisions after fertilization, and typically causes early spontaneous miscarriage.
Triploidy pregnancies can often go full-term, although the baby rarely survives beyond a few days. An NIPT test, confirmed by a test of the fetal genetic material in the amniotic fluid, can detect this early in the pregnancy.
Structural aberrations
Chromosomes can get damaged during the production of eggs and sperms, and during the transport of sperms from the testicles to the eggs. There are many different types of structural aberrations.
1) Deletions
Deletions are when a part of a chromosome is missing. This can cause a loss of genes required for embryonic growth or development.
2) Duplications
Duplication is when a part of the chromosome is duplicated, increasing the copy number of genes in the duplicated region.
3) Insertions
A part of a chromosome can be deleted from one place and inserted into another in the genome. Within an individual, this typically does not cause a gain or loss of genes. But when the individual has children, their children may inherit the chromosome with the deletion or insertion, causing miscarriage or congenital defects.
4) Inversions
When part of a chromosome breaks off and reattaches backward, the chromosome has an inversion. This does not cause a loss of genes but in some cases, if the breakage occurs in the middle of a gene, it can impact gene function.
Chromosomes with inversions may interfere with meiosis, the cell division that produces eggs and sperms. As a result., parents with chromosomal inversions may be more likely to produce eggs or sperms with broken or translocated chromosomes.
5) Ring chromosomes
When the cell attempts to repair the broken chromosomes, sometimes it rejoins the wrong ends, resulting in a ring chromosome11. Ring chromosomes typically occur in an error during the production of sperms or eggs, or after fertilization. However, in rare cases, ring chromosomes can be present in all cells of the parents and transmitted to the children12.
6) Translocations
A translocation is when a part of a chromosome breaks off and rejoins another chromosome. There are two types of translocations: balanced and imbalanced1314.
In a balanced translocation, two chromosomes exchange parts, resulting in no gain or loss genes.
The notations such as t(13, 14) means that the long arms of chromosomes 13 and 14 fuse. t(13,14) is the most common balanced chromosomal translocation in humans15, although other translocations between chromosomes 13, 14, 15, 21, and 22 are also found.
In an imbalanced translocation, a piece of one chromosome breaks off and attaches to another chromosome.
These translocations typically don’t cause any gain or loss of genes, so they can be silent, resulting in no health problems. However, when people with translocations become parents, the embryo or child can inherit one of the chromosomes with translocations. There are 3 possibilities that the child may inherit:
- entirely normal chromosomes, thus developing normally.
- both the source and the receiving chromosomes in a translocation, thus developing normally.
- one of the abnormal chromosomes but not the other, often resulting in a miscarriage or developmental problems. For example, a person inheriting an extra part of chromosome 21 translocated onto another chromosome can develop Down’s syndrome.
60 – 70% of parents who are carriers of balanced chromosomal translocations can have successful pregnancies and healthy children, depending on the specific translocations1617. Whereas, with unbalanced or abnormal chromosomes, the rates of live births are under 1% 1819. If you are a carrier, your doctor may refer you to a genetic counselor. In addition, in vitro fertilization with preimplantation genetic testing may significantly improve your chance of live birth20.
7) Other gene-specific mutations
Previously, the main method of choice for assessing chromosomal anomalies was karyotyping. A karyotype can only identify structural anomalies over 5 million base pairs in size. Recently, more advanced techniques such as chromosomal microarray and next-generation sequencing have become available. These technologies can better identify smaller genetic mutations as potential causes of recurrent pregnancy losses. These include smaller changes in copy number of genes, deletions, and even mutations involving one single nucleotide.
Deletions in the DiGeorge region of chromosome 22 (22q11.2) may cause recurrent miscarriages, especially in the 2nd trimester21. These abnormalities are too small to be detectable on a karyotype.
What causes chromosomal anomalies?
Chromosome anomalies are not your fault. Once the miscarriage occurs due to a chromosomal problem in the embryo, there is nothing you can do to stop the miscarriage. However, understanding why a miscarriage occurs may give you closure and help you make the right decisions to reduce the risk of future miscarriages. If you have recurrent miscarriages, testing the product of conception with microarray and the parents with karyotyping can help you decide on the best ways to prepare for the next pregnancy.
Risk factors for a chromosomal anomalies include:
- Increased parental age, over 35 for mothers and 40 for fathers, increases the risk of trisomies22.
- Parental carrier status – balanced translocations are found in 3 – 5% of couples with recurrent pregnancy loss, compared to 0.2% in the general population2324. Therefore, if you struggle with multiple recurrent miscarriages, you may want to ask your doctor about getting screened for chromosomal translocation carrier status.
- Sperm DNA fragmentation may result in embryos with chromosomal aberrations and genetic mutations that cause miscarriage25.
- Exposure to substances that cause birth defects (teratogens) – some medications, chemicals, or health conditions can contribute to DNA damage. These may include:
- Radiation
- Diabetes
- Elevated homocysteine
- Medications such as methotrexate and colchicine
- Chemotherapy drugs
Should you get genetic testing?
Genetic screening is a powerful tool for pregnancy planning, but not everyone wants to know the information they provide or is willing to act on the result. As prospective parents, you should have options for screening, testing, and dealing with the result in a comprehensive and tolerant way.
Women should be offered but not obliged to do screening or diagnostic tests26. You have every right to decline the genetic test and continue the pregnancy without knowing if your child has a genetic anomaly.
If you don’t wish to have your decision shaped by the result of genetic testing, you also have the complete right to take no measures27. You must be able to make an independent informed decision rather than be pressured by health care professionals or society.
On the other hand, if the couple or the mother wishes not to continue the pregnancy upon finding a genetic defect in the fetus, they need to have medical support. These options may be considered to end the suffering of the child, prevent possible life-threatening complications of a natural miscarriage that will occur, and allow the couple to try again sooner.
There are some bioethical considerations with genetic testing, especially with commercial tests. It can lead to their misuse and further discrimination against people with genetic diseases. For example, genetic tests can tell the gender of the child and sometimes identify non-paternity. However, wise screening may identify causes of miscarriage, stillbirth, and congenital defects.
For prospective parents who know ahead of the pregnancy that they carry a genetic aberration, independent of whether the recessive gene or balanced translocation is in question, egg or sperm donation should be an option.
If the mother is the carrier of a genetic mutation that leads to nonviable embryos, egg donation or surrogacy is an option. If the father is the carrier of the damaged genetic material, sperm donation may be considered.
This might be a complicated concept for future parents to grasp, as the child is not completely genetically theirs, but it might enable a successful pregnancy experience and compromise for parenting desire. The decision ought to be entirely on the parents and they should have enough time to ponder and make up their mind within the legal frame of their country.
Conclusion
Chromosomal and genetic mutations are leading causes of miscarriage. However, if you’ve had more than one miscarriage, you or your partner should be screened for carrier status for these genetic issues. If one of you is a carrier, a genetic counselor can help you understand your options. Also, in vitro fertilization with preimplantation genetic testing can select for the embryo without genetic problems.
If neither of you is a carrier, consider testing the product of conception for genetic anomalies. If you’ve had at least one miscarriage due to a genetic problem, investigate lifestyle factors that can lead to spontaneous genetic issues. Whereas, if the genetic test came back normal, it would be time to investigate other causes.
There are also genetic tests that can screen for potential genetic issues in the embryo during pregnancy. To learn more about these, check out our genetic testing article.
Next Steps to Consider
- If you have not already, reach out to your doctor about karyotype or more advanced genetic testing
- This topic of genetic testing and medical abortions can bring up difficult moral and ethical issues; it is important to have the conversations in order to reach the decision best for you
- It is important to understand risk factors for chromosomal anomalies, but also keep in mind healthy pregnancy is typically possible after miscarriage due to genetic issues
References



0 Comments